Cervical and ovarian cancers are both common cancers affecting the female reproductive system. Cervical cancer is the 4th most commonly diagnosed cancer in women worldwide, while ovarian cancer is the 8th most common.
Cervical Cancer:
The cervix is a disc-like structure that sits at the top of the vaginal canal and the bottom of the uterus. Cervical cancer occurs when the cells of the cervix develop into cancerous cells. The primary cause of cervical cancer is Human Papillomavirus (HPV). HPV is a common sexually transmitted infection, which almost all sexually active people encounter at some point in their lives. In most cases, the immune system clears the infection on it’s own. A persistent infection can cause abnormal cells to grow, which may progress to cervical cancer.
Since HPV is sexually transmitted, sexual activity can increase your risk of cervical cancer. A common misconception is that HPV spreads through sexual intercourse only, but it can also be transmitted through any genital-to-skin contact, including oral sex. While becoming sexually active at a younger age or having many sexual partners increases the likelihood of exposure to the virus, it only takes one exposure to potentially become infected.
Other risk factors for cervical cancer include smoking, giving birth multiple times and any immune-lowering condition such as HIV or other sexually transmitted infections, like chlamydia. Having an immune-lowering condition makes it more likely for an HPV infection to persist and become cervical cancer.
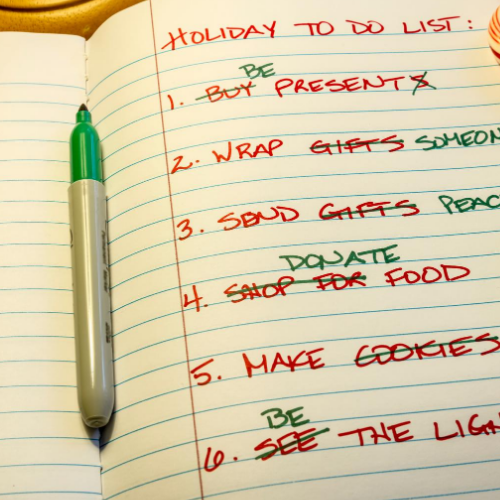
If detected early, cervical cancer is typically very treatable. Therefore, regular screening is vital. Screening is done with a Pap test, which includes a pelvic exam to collect a sample of cervical cells. A Pap test will detect if there are abnormal cervical cells, and further testing determines the cause. Some regions are beginning to use more sensitive Pap tests that specifically look for HPV. To learn more about cervical cancer screening programs in your area, reach out to your local public health agency or your family doctor. Most screening programs with a Pap test begin between 20 and 30 years of age, in sexually active people, and are recommended every 3-5 years.
Currently, there are 6 vaccines available worldwide for HPV. The WHO recommends vaccinating girls ages 9-14, before they become sexually active. In some countries, boys are starting to be vaccinated against HPV as well. HPV vaccines are also available to people over 14 if they wish. Consult your doctor about the benefits and risks associated with HPV vaccines for your personal health.
Ovarian Cancer:
The ovaries are the organs that sit on either side of the uterus and are responsible for the maturation of eggs and producing the hormones, estrogen and progesterone. Ovarian cancer occurs when cancerous cells develop on or within the ovaries. Several risk factors are associated with ovarian cancer, including:
• Family history of ovarian cancer
• Certain genetic conditions
• Older age (most diagnoses occur post-menopause)
• Using hormone replacement therapy for over 5 years
• Smoking
• Being overweight
• Living a sedentary lifestyle
Some research indicates that a history of breast cancer may increase your risk of ovarian cancer. This could be because they have some of the same risk factors, such as, starting your period before age 11, starting menopause after age 55, never being pregnant, and some gene mutations. There are currently no formal screening programs in place for ovarian cancer. You can discuss your risk factors and any symptoms with your doctor to decide if further testing is required.
Symptoms:
Cervical and ovarian cancer can cause many of the same symptoms. It is important to note that these symptoms usually result from more common, less severe conditions and having one or more of these symptoms does not mean cancer is present. Some symptoms of cervical and ovarian cancer include:
• Abnormal vaginal bleeding (after menopause, between periods, after intercourse, heavy menstrual bleeding)
• Abnormal change in or increased amount of vaginal discharge
• Changes to urination such as increased urgency and frequency to urinate
• New onset constipation
• Pain during intercourse
• Unintentional weight loss
• Night sweats
• Lump felt in abdomen or pelvic area (specific to ovarian cancer)
Speak to your doctor if you notice any of these symptoms. While they may not be cancer-related, it is important to investigate and treat the cause.